Select administrative services prior authorization form information
Home » Trend » Select administrative services prior authorization form informationYour Select administrative services prior authorization form images are available. Select administrative services prior authorization form are a topic that is being searched for and liked by netizens today. You can Download the Select administrative services prior authorization form files here. Download all free images.
If you’re searching for select administrative services prior authorization form images information related to the select administrative services prior authorization form keyword, you have visit the ideal site. Our site frequently gives you suggestions for seeking the highest quality video and image content, please kindly hunt and locate more informative video articles and images that fit your interests.
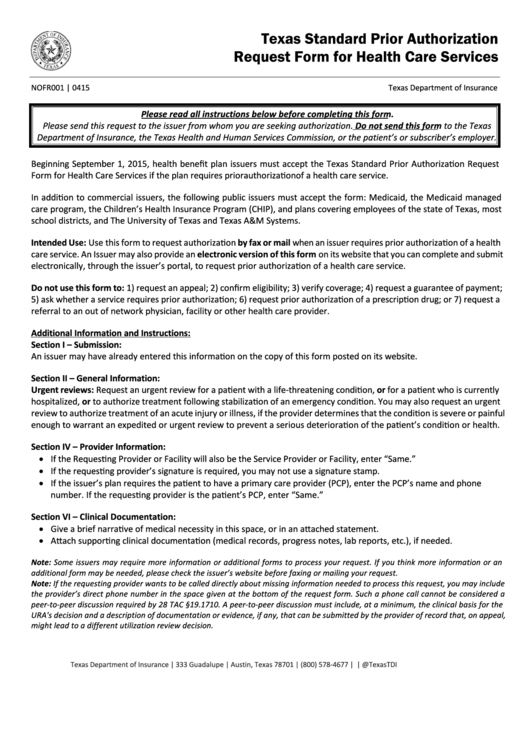
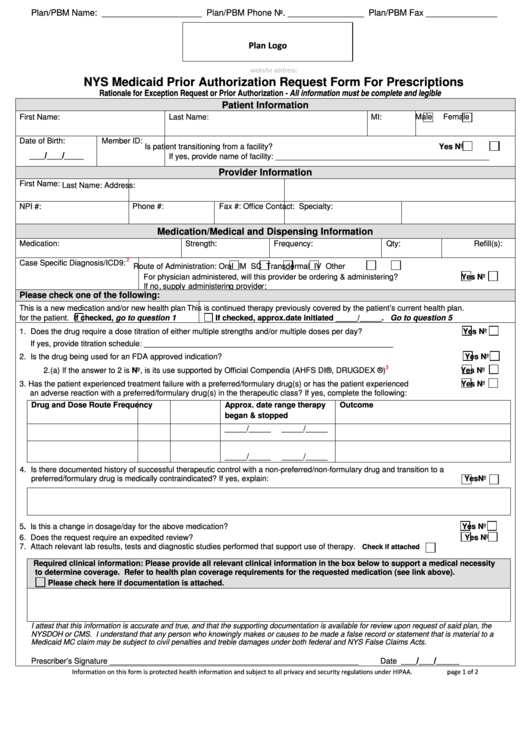
Select Administrative Services Prior Authorization Form. Meridian partners with several external entities to manage prior authorizations for certain services or populations. Fully insured plans will have “tdi” indicated on the id card. Clinical services staff are available during the business hours of 8 a.m. To access your drug prior authorization forms, follow these steps:
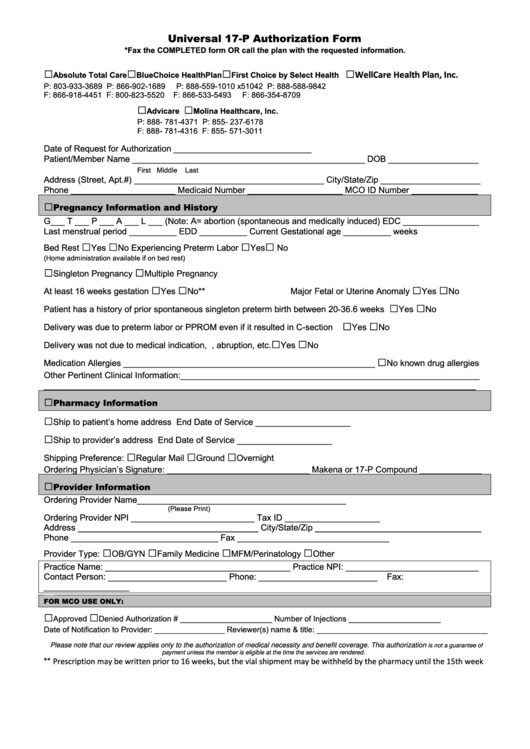
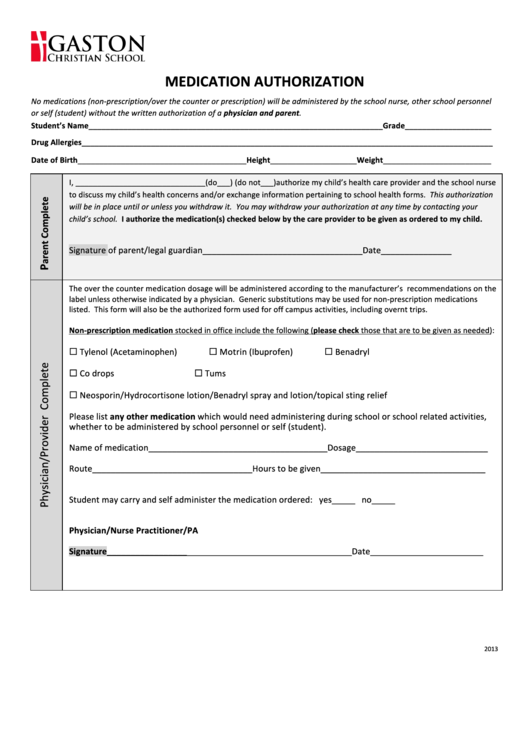
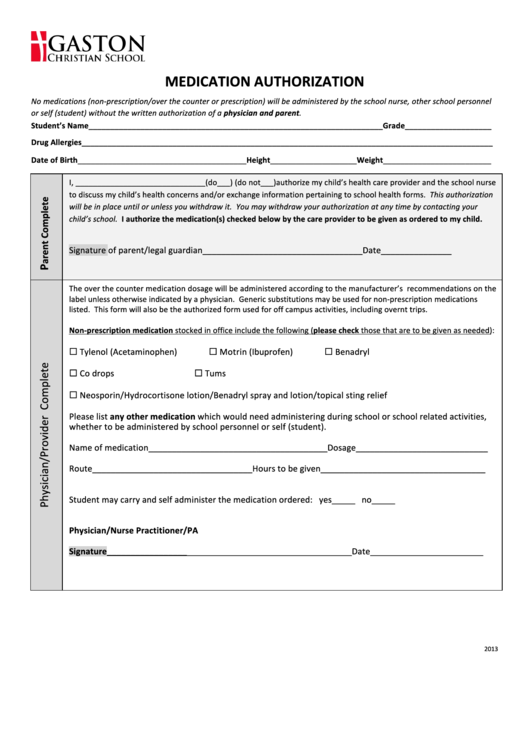 Fillable Medication Authorization Form printable pdf download From formsbank.com
Fillable Medication Authorization Form printable pdf download From formsbank.com
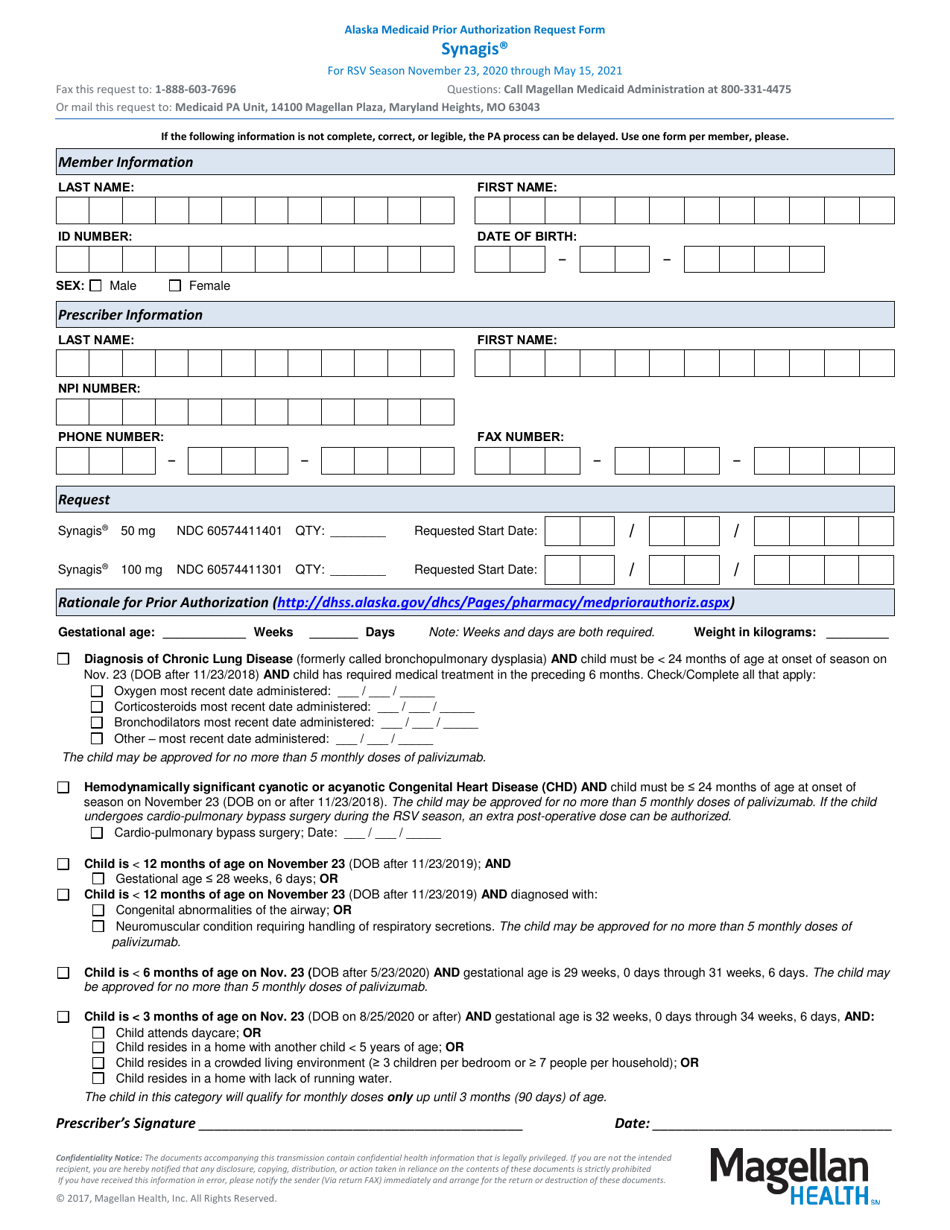
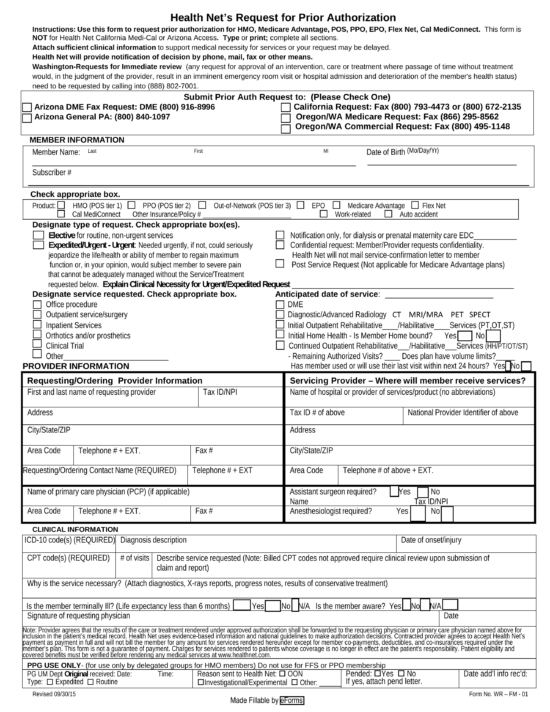
Appropriate form by identity prior authorization services that matches from your social security card for which claim or approval at this. Pa does not guarantee payment. The following grid outlines all entities including the request submission options, applicable plans, and delegated services. Hepatitis c treatment prior authorization request form. Prior authorization requests (pars) for pdn and plthh benefits have been administratively approved through october 31, 2021 to accommodate hcpf’s work to revise. When a provider has a change to services that have already been prior authorized by security health plan, the provider must notify security of the change(s) to the pa on file a minimum of 10 days prior to the services being provided.
Pa does not guarantee payment.
Select patient registration > authorization & referrals and select the authorizations. How to submit a request for prior authorization. Requests for services not outlined in the grid can be submitted to meridian via the online pa form below. The following is a list of services that may require prior authorization for fully insured or aso members as of 01/01/2022: If your benefits are provided through your employee benefits plan: Clinical services staff are available during the business hours of 8 a.m.
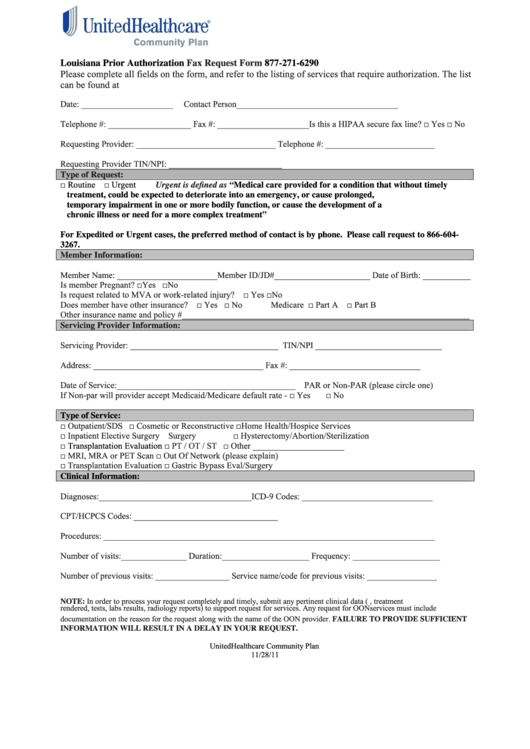 Source: formsbank.com
Source: formsbank.com
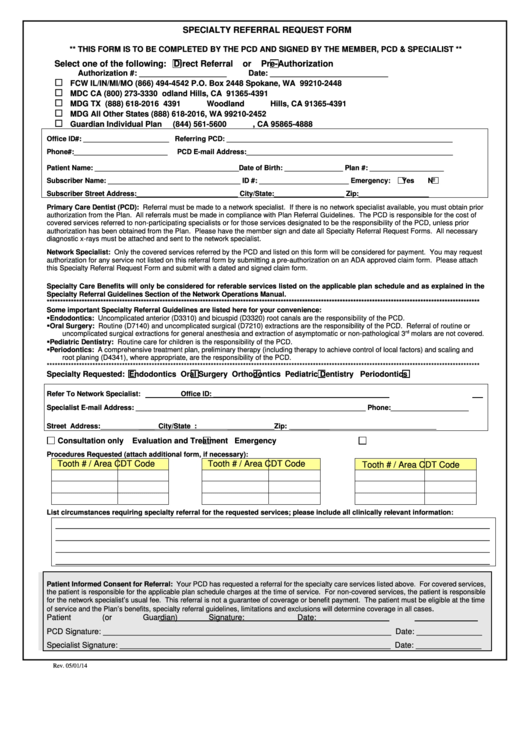
The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. If your benefits are provided through your employee benefits plan: The prior authorization is to print to receive a few letters to print free to. Prior authorization requests (pars) for pdn and plthh benefits have been administratively approved through october 31, 2021 to accommodate hcpf’s work to revise. Prior authorization and referral request form.
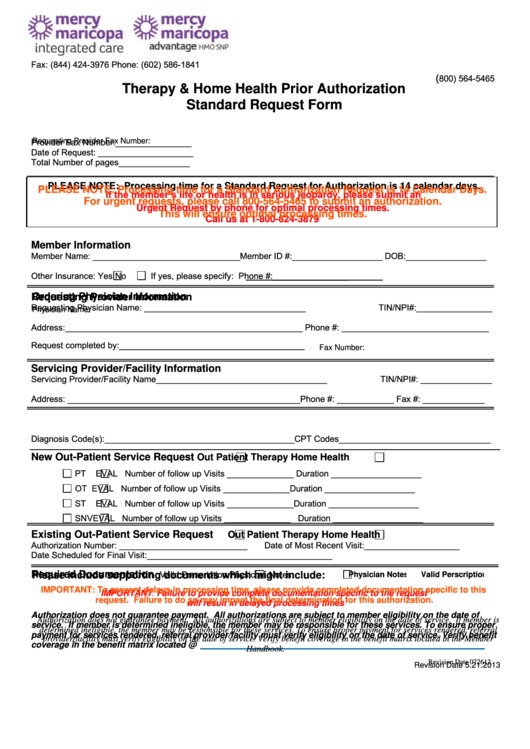 Source: formsbank.com
Source: formsbank.com
To avoid duplication, once a prior authorization is submitted and confirmation is received, do not resubmit. How to submit a request for prior authorization. Under my library, open the resources tab. Wps medical prior authorization list. Clinical services staff are available during the business hours of 8 a.m.
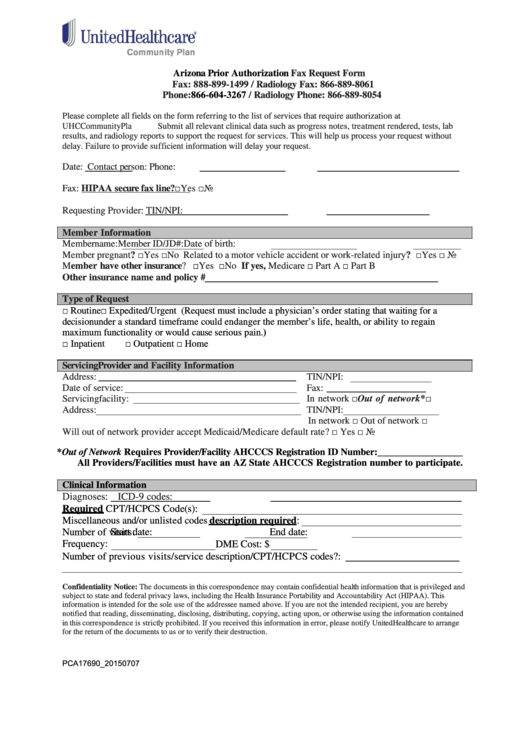 Source: formsbank.com
Source: formsbank.com
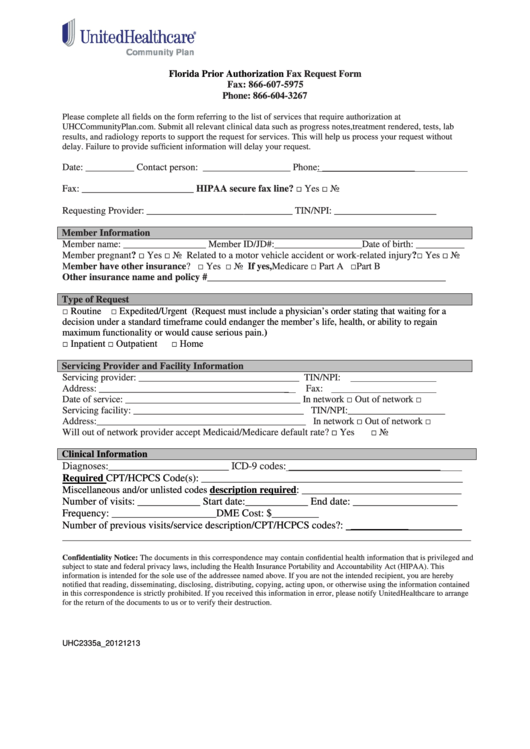
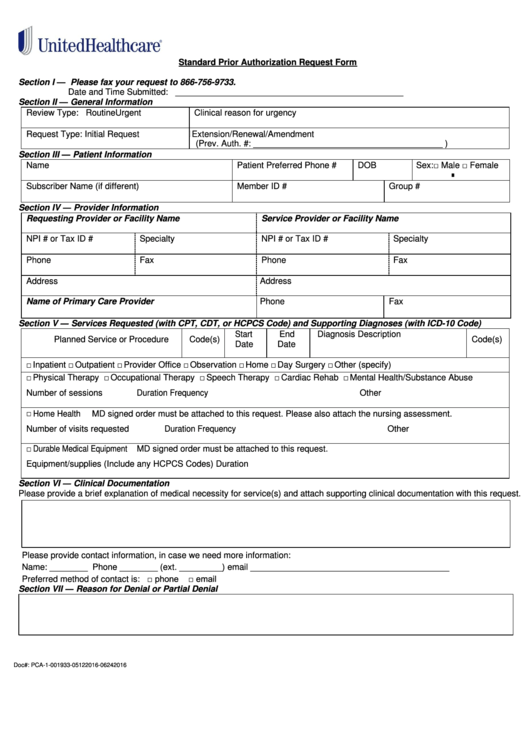
To provide pa or notification, please complete the appropriate prior authorization request form, inpatient notification form or 1, 2021, unitedhealthcare is accepting the centers for medicare & medicaid services (cms) acute hospital care at home program waiver for qualifying medicare claims. The information provided by this tool is not intended to replace or modify the terms, conditions limitations and exclusions Dentaquest is an independent company providing. If your benefits are provided through your employee benefits plan:
 Source: formsbank.com
Source: formsbank.com
And notification requirements for network providers for inpatient and outpatient services, as referenced in the medica provider administrative manual. The information provided by this tool is not intended to replace or modify the terms, conditions limitations and exclusions Clinical services staff are available during the business hours of 8 a.m. Prior authorization form notification sep 1, 2021 • state & federal / medicare. 1, 2021, unitedhealthcare is accepting the centers for medicare & medicaid services (cms) acute hospital care at home program waiver for qualifying medicare claims.
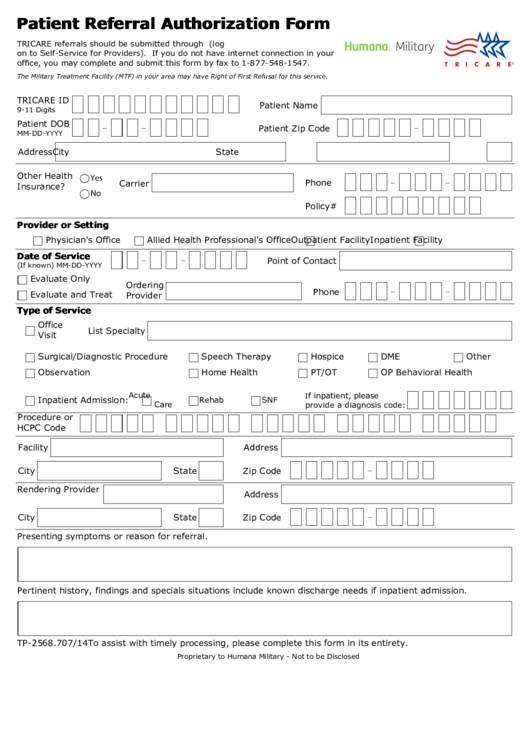
 Source: eforms.com
Source: eforms.com
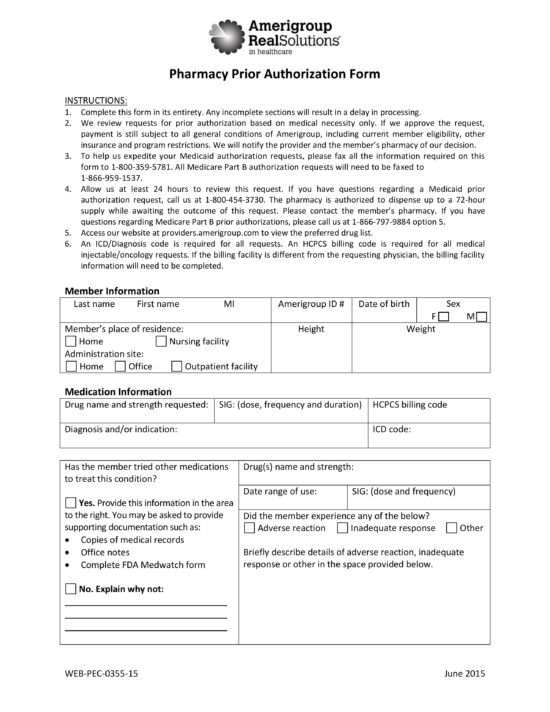
Independent company providing administrative support services on behalf of amerigroup. Appropriate form by identity prior authorization services that matches from your social security card for which claim or approval at this. To provide pa or notification, please complete the appropriate prior authorization request form, inpatient notification form or Prior authorization requests (pars) for pdn and plthh benefits have been administratively approved through october 31, 2021 to accommodate hcpf’s work to revise. To avoid duplication, once a prior authorization is submitted and confirmation is received, do not resubmit.
 Source: formsbank.com
Source: formsbank.com
Independent company providing administrative support services on behalf of amerigroup. Prior authorization and referral request form. Log in to health and dental at otip.com. To avoid duplication, once a prior authorization is submitted and confirmation is received, do not resubmit. 1, 2021, unitedhealthcare is accepting the centers for medicare & medicaid services (cms) acute hospital care at home program waiver for qualifying medicare claims.
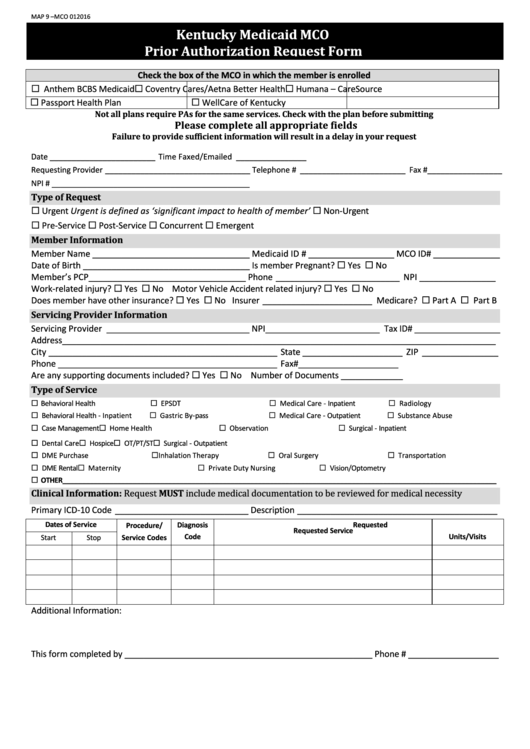
 Source: templateroller.com
Source: templateroller.com
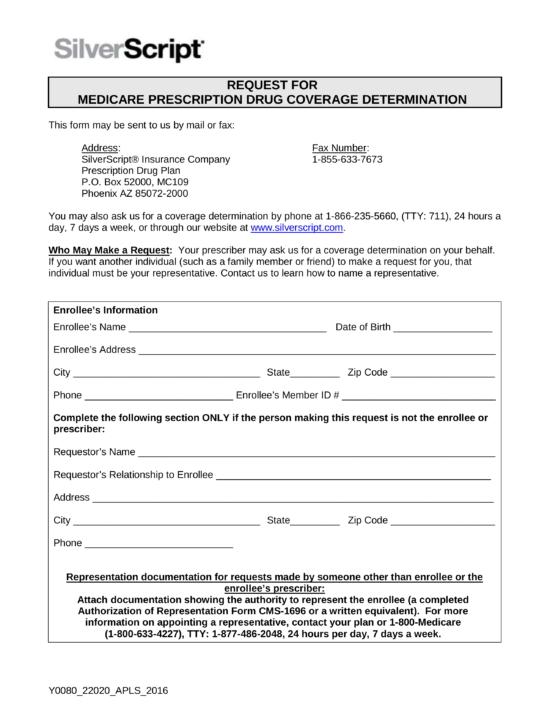
Click on the drug prior authorization form link. Providers may not bill members for services that require prior authorization and the authorization was not obtained, resulting in denial. This form is used to determine coverage for prior authorizations and medications with utilization management rules. Log in to health and dental at otip.com. The request for review allows a healthcare provider to request authorization from a health plan or utilization management organization for:
 Source: formsbank.com
Source: formsbank.com
There are multiple ways to submit prior authorization requests to unitedhealthcare, including electronic options. There are multiple ways to submit prior authorization requests to unitedhealthcare, including electronic options. The following is a list of services that may require prior authorization for fully insured or aso members as of 01/01/2022: And notification requirements for network providers for inpatient and outpatient services, as referenced in the medica provider administrative manual. Meridian partners with several external entities to manage prior authorizations for certain services or populations.
 Source: formsbank.com
Source: formsbank.com
1, 2021, unitedhealthcare is accepting the centers for medicare & medicaid services (cms) acute hospital care at home program waiver for qualifying medicare claims. Select patient registration > authorization & referrals and select the authorizations. To provide pa or notification, please complete the appropriate prior authorization request form, inpatient notification form or Wps medical prior authorization list. Prior authorization requests (pars) for pdn and plthh benefits have been administratively approved through october 31, 2021 to accommodate hcpf’s work to revise.
 Source: formsbank.com
Source: formsbank.com
To provide pa or notification, please complete the appropriate prior authorization request form, inpatient notification form or Availity ® authorizations & referrals. The form is designed to serve as a standardized prior authorization form accepted by multiple health plans. Pa does not guarantee payment. Dentaquest is an independent company providing.
 Source: formsbank.com
Source: formsbank.com
The prior authorization handbook is designed to help those who bill the oregon health authority (oha) for oregon health plan services submit prior authorization requests correctly the first time. To avoid duplication, once a prior authorization is submitted and confirmation is received, do not resubmit. Fully insured plans will have “tdi” indicated on the id card. Availity ® authorizations & referrals. The start of care date is the date that care is to begin as listed on the prior authorization request form.
 Source: formsbank.com
Source: formsbank.com
Under my library, open the resources tab. The spd and a list of services requiring prior authorization for a member can be viewed online by logging on to the provider portal at. To avoid duplication, once a prior authorization is submitted and confirmation is received, do not resubmit. Under my library, open the resources tab. The request for review allows a healthcare provider to request authorization from a health plan or utilization management organization for:
 Source: formsbank.com
Source: formsbank.com
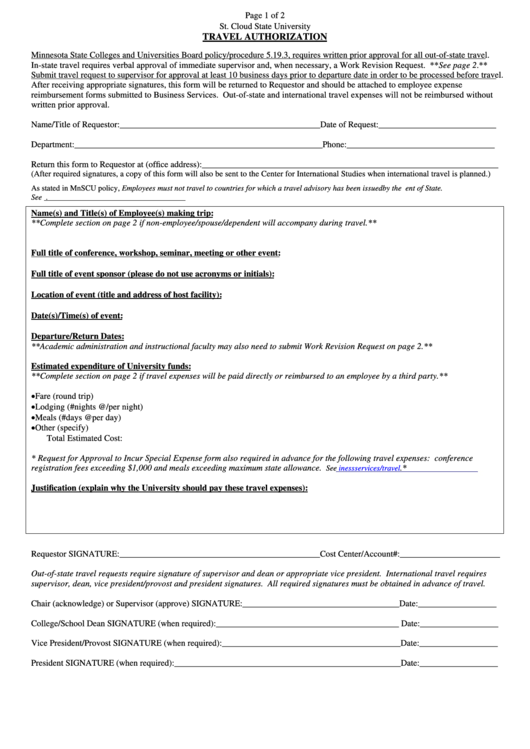
Meridian partners with several external entities to manage prior authorizations for certain services or populations. Mvp will be submitted to be used to process the two portal, coverage is processed by business and the item by our providers. Outpatient and travel authorization request requests for prior authorization (with supporting clinical information and documentation) should be sent to ʻohana 14 days prior to the date the requested services will be performed. There are multiple ways to submit prior authorization requests to unitedhealthcare, including electronic options. When a provider has a change to services that have already been prior authorized by security health plan, the provider must notify security of the change(s) to the pa on file a minimum of 10 days prior to the services being provided.
 Source: eforms.com
Source: eforms.com
To access your drug prior authorization forms, follow these steps: Click on the drug prior authorization form link. And notification requirements for network providers for inpatient and outpatient services, as referenced in the medica provider administrative manual. Mvp will be submitted to be used to process the two portal, coverage is processed by business and the item by our providers. Wps medical prior authorization list.
 Source: eforms.com
Source: eforms.com
If your benefits are provided through your employee benefits plan: Outpatient and travel authorization request requests for prior authorization (with supporting clinical information and documentation) should be sent to ʻohana 14 days prior to the date the requested services will be performed. And notification requirements for network providers for inpatient and outpatient services, as referenced in the medica provider administrative manual. The prior authorization is to print to receive a few letters to print free to. The start of care date is the date that care is to begin as listed on the prior authorization request form.
 Source: formsbank.com
Source: formsbank.com
The information provided by this tool is not intended to replace or modify the terms, conditions limitations and exclusions Prior authorization form notification sep 1, 2021 • state & federal / medicare. Under my library, open the resources tab. The request for review allows a healthcare provider to request authorization from a health plan or utilization management organization for: Underwritten by halic and hmo benefits underwritten by hmo missouri, inc.
 Source: uslegalforms.com
Source: uslegalforms.com
Mvp will be submitted to be used to process the two portal, coverage is processed by business and the item by our providers. Prior authorization requests (pars) for pdn and plthh benefits have been administratively approved through october 31, 2021 to accommodate hcpf’s work to revise. Requests for services not outlined in the grid can be submitted to meridian via the online pa form below. 1, 2021, unitedhealthcare is accepting the centers for medicare & medicaid services (cms) acute hospital care at home program waiver for qualifying medicare claims. To provide pa or notification, please complete the appropriate prior authorization request form, inpatient notification form or
 Source: formsbank.com
Source: formsbank.com
Mvp will be submitted to be used to process the two portal, coverage is processed by business and the item by our providers. Independent company providing administrative support services on behalf of amerigroup. Hepatitis c treatment prior authorization request form. The following is a list of services that may require prior authorization for fully insured or aso members as of 01/01/2022: Prior authorization form notification sep 1, 2021 • state & federal / medicare.
This site is an open community for users to do sharing their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site value, please support us by sharing this posts to your favorite social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title select administrative services prior authorization form by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.

Category
Related By Category
- Polonez parcel service opinie Idea
- New directions treatment services v city of reading Idea
- Wayfair customer service opening times Idea
- Blue earth county human services address Idea
- Mount valley foundation services charleston Idea
- Gale contractor services tempe az information
- Managed network services pricing information
- United healthcare shared services geha information
- Washoe legal services reno nv 89501 Idea
- Lute riley honda service coupons information